Table of Contents
Body Mass Index – Definition
Body Mass Index – A key index for involving weight to height. Abbreviated BMI. BMI is a person’s weight in kilograms (kg) divide by their size in meters square. The National Institutes of Health (NIH) now defines average weight, overweight, and obesity according to BMI slightly than the traditional height/weight charts.
Obesity is a BMI of 30 or more for either sex
A very well-built person might have a high BMI deprived of health risks.
Assessing Your Weight and Health Risk with Body Mass Index
Body Mass Index (BMI)
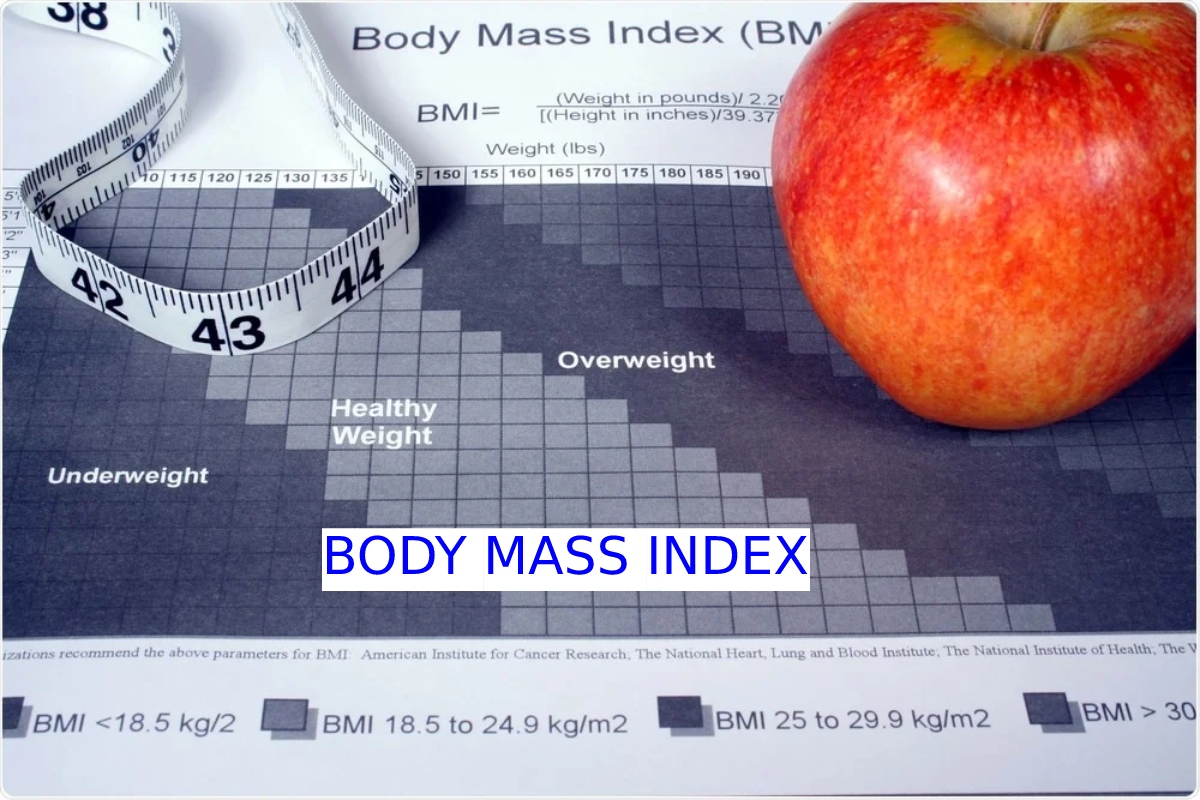
BMI is a useful measure of overweight and obesity. It is designed for your height and weight. BMI estimates body fat and is a suitable device for your risk for diseases with more body fat. The higher your BMI, the more complex your risk for specific conditions such as heart disease, high blood pressure, type 2 diabetes, gallstones, breathing difficulties, and positive cancers.
Although BMI can be used for most men and women, it does have some limits:
It might overrate body fat in athletes and others with a muscular build.
It may undervalue body fat in older persons and others who have lost muscle.
Use the BMI Adder or BMI Tables to approximation your body fat. The BMI score income the following:
Waist Circumference
Measuring waist circumference helps screen for likely health risks with overweight and obesity. If most of your fat is about your waist rather than at your hips, you’re at a higher risk for heart sickness and type 2 diabetes. This risk increases with a waist size better than 35 inches for women or greater than 40 inches for men. To correctly measure your waist, stand and place a tape around your middle, just above your hipbones.
The table Risks of Obesity-Associated Sicknesses by BMI and Waist Circumference provides you with an idea of whether your BMI joint with your waist boundary growths your risk for evolving obesity-associated diseases or conditions.
Risk Factors for Health Topics Accompanying with Obesity of Body Measure Index
Along with being overweight or obese, the following situations will put you at greater risk for heart disease and other conditions:
For people who are careful obese or overweight (BMI of 25 to 29.9) and have two or more risk issues, it is suggested that you lose weight. Individuals who are overweight, do not have a high stomach measurement, and have fewer than two risk factors may need to prevent extra weight gain rather than lose weight. Even a slight weight loss (between 5 and 10 per cent of your current weight) will help lower your risk of evolving diseases associated with obesity.
Exchange to your doctor to see whether you are at an improved risk and whether you must lose weight. Your doctor will assess your BMI, waist measurement, and other risk factors for emotional illness.
Fatness as a Personal or Society Issue
Traditionally, a person’s obesity has been defined personally and socially. However, this isn’t easy to quantify. Each individual has their perception of how fat they should be. As specified above, this often depends on a general concept of societal norms or is due to peer pressure.
For example, in Western societies. young women are often concerned about their body image and most consider themselves too fat. Even though they are well within population-based references. This is due to societal concepts of an ideal degree of fatness and thinness being a goal promulgated by the fashion industry and armour-plated by commercial advertising.
Although poorly described or quantified at a social level, there is also a degree of fatness outside which a person generally is considered to be unacceptably fat. That is there is an ill-defined threshold at which a person is labelled as being “fat” or “obese.” However, it is founded on the “I can’t define it, but I know it when I see it” concept. In accumulation, implicit in this context is that the location of the extra fat plays a role, as does a person’s age.
It is much more suitable to be “overweight” when old than young. Also, mainly in women, the accumulation of fat in certain body areas is careful much more acceptable than in other areas. For example, the truncal expansion would be considered to be less satisfactory than the accumulation of fat in the peri pelvic and thigh areas as well as in the breast area1.
Discrimination begins in childhood and results in profound emotional scars. The social penalties of being “too fat” are severe. Societal discrimination limits career choices. And many career paths close to those considered too fat. Also, social stigmatization often impairs a person’s ability to express their intellectual and other talents; that is, they become underachievers.
In addition, the potential pool of mates is because of their unattractiveness. Thus, obese people tend to marry other heavy people and, by the way, produce obese children.
Problems with the Wt. Body Mass Index
Early on, tall people had a lower death rate than short people7,8,13 with the same Wt/Ht ratio. It also was known that a person’s height in general and leg length. Inexact could touch the calculates body mass for height.
A person’s bony surround, that is, jaw mass also might touch the clarification of this ratio. In general, it reflected whether one was only just or approximately built. The strategy was to develop pictures of body build. That is charts of weight/height independent of these variables. The overall goal was to have a similar supply of Wt/Ht at each extreme level.
Although not the implicit goal in evolving these tables is a person’s fat form as a proportion of their total mass. irrespective of their height or frame size.
14 Labors to adjust for frame size by categorizing people as small-medium. Estimation of frame size attempt using some quantities. Including shoulder width, elbow width, knee width. Ankle width and so on15 None of these were extensive. Nevertheless, frame size based on prod width includes in the Metropolitan Life weight/height tables,7,10.
BMI as a Cause of Body Fat Mass
A particular tricky with BMI as an index of obesity. Is that it does not separate between lean body mass and body fat mass. That is, a person can have a high BMI but still have a very low-fat group and vice versa.39,41–46.
From an anatomical and metabolic perspective. Obesity should refer to an excessive accumulation of body fat. Upon these grounds, the exactness of the BMI as a cause of body fat mass repeatedly grilled,16,39–41,46–48 because it has limits in this respect. Gender, age, ethnic group, and leg distance are essential variables.45.49–55 It must note that in population-based education. Women usually have a BMI lower than that in men, even though their fat mass relative to their body build or BMI is considerably greater.
Methods of Estimating Body Fat Mass and Position of the Fat
At present, simple, accurate measuring per cent of body fat and, in particular, body fat in different fat depots are not available. The indirect methods currently used for estimating the total per cent of body fat include underwater weighing, an air displacement and density resolve using a Bod Pod.
A bioelectrical impedance analyzer, and a determination of the isotopically labelled water mass. In the past, resolution of the total body radioactive potassium and thus absorbing. Tissue mass to estimate lean body mass and by difference, the fat mass.86
BMI and Morbidity and Mortality
Studies to evaluate the risk for mortality in the different groups of BMI. It also regards specific etiologists for mortality risk. However, as with its use to estimate per cent of body fat, it is a relatively simple method.
Even when some comorbidities consider. The association of mortality rates with BMI often does not consider such factors as family history of diabetes. Hypertension coronary heart disease, metabolic. Syndrome, dyslipidaemias. Familial longevity or the family prevalence carcinomas and so on. Recently it report that genetic variants account for more than 50% of susceptibility to coronary artery disease.9
Conclusion
The current BMI classification system is also misleading. The effects of body fat mass on mortality rates. The role of fat distribution in predicting medically significant. Morbidities and mortality risk by the use of the BMI. Also, numerous comorbidities, lifestyle issues, gender, ethnicities.
Medically significant familial-determined mortality effectors. The duration of time one spends in specific BMI categories. And the expected accumulation of fat with ageing is likely to sign. Affect the interpretation of BMI data. Particularly concerning morbidity and mortality rates.
Such confounders and the known clustering of obesity in families. The decisive role of genetic factors in the development of obesity, the location in which excessive fat accumulates. Its role in the development of type 2 diabetes and hypertension.